Did Infamous Tuskegee Study Cause Lasting Mistrust of Doctors Among Black Americans?
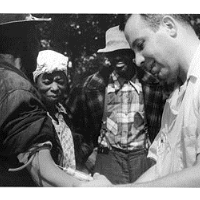 Doctor draws blood from a Tuskegee "test subject" (photo: Wikipedia)
Doctor draws blood from a Tuskegee "test subject" (photo: Wikipedia)
By Aaron E. Carroll, New York Times
There is no question that the Tuskegee study is one of the most horrific examples of unethical research in recent history. For 40 years, ending in 1972, members of the U.S. Public Health Service followed African-American men infected with syphilis and didn’t treat them (although they told some men they did) so that they could see the disease take its course.
There’s also no question that this experiment shook the foundations of trust between Americans, especially black Americans, and the medical establishment. A new paper argues that this wound was so severe that it led older African-American men to avoid care, leading to a decrease in life expectancy of 1.4 years, accounting for about a third of the discrepancy in life expectancy between black and white men by 1980.
While few question that there are racial disparities in life expectancy or health care, and no one questions the utter lapse in ethics of the Tuskegee experiment, we should still be wary in connecting the two without a clear causal link. To do so compounds mistrust in the health care system.
The recent study (pdf), published by the National Bureau of Economic Research as a working paper (meaning it has not yet undergone full peer review), combined data on mistrust of doctors from the General Social Survey, health care utilization from the National Health Interview Survey and mortality data from the Centers for Disease Control and Prevention. They then used sophisticated statistical techniques to test for how these three variables might be related.
The researchers found that after 1972, when much of the truth behind Tuskegee was revealed, mistrust among African-Americans toward the medical profession spiked. They found that use of the health care system fell, and that mortality increased years later. They hypothesized that each factor led to the next: The news caused African-Americans to doubt the health care profession was interested in their well-being, they stopped going to the doctor, and this led to earlier deaths. They even showed that the closer you lived to Macon County, Alabama, where the study took place, the greater the effect.
This is an impressive paper. Although establishing causality in a study like this is nearly impossible, the authors anticipated many potential critiques. They did tests to account for migration. They looked at other measures of mortality. They even performed the geographic analysis from all 50 states to show that centering it on Macon County yielded different results than in most other places.
Still, I think there are limitations that argue against making a causal leap. The biggest is that this effect was seen in black men, but not in black women. The authors posit that this might be because women are forced to engage in the health care system (during childbirth) in ways that men are not, and that this led to a greater level of trust. But this dynamic isn’t assured. You can have a baby and still mistrust the health care system enough to avoid screening later in life. I find it hard to believe that black men and women didn’t share their fears and mistrust of the system with each other.
A second concern involves geography. The analysis looked at the distance from Macon County to show that those closer had fewer doctor and hospital visits and greater mortality than those outside the circle. If you look at the map they provide, a circle around that point almost perfectly encapsulates the Deep South. Disparities in care might have arisen in that region for any number of reasons, and blame can’t be assigned entirely to the Tuskegee study.
A third concern involves the arrow of causality. The authors argue that their evidence supports a theory explaining that mistrust causes less use of doctors, which causes higher mortality. Given what we know of disparities in care in the United States, it still seems possible that the medical system itself could have been throwing up barriers. It’s easy to believe that black men had a harder time getting care than white men, or they might have been subtly turned away or dismissed, which also would lead to less use and perhaps higher mortality.
Let me be clear about a few things. There is no reason to believe that the differences in use or outcomes aren’t real. They’re both terrible, and they both need fixing. I also don’t believe the statistics are flawed, or that the researchers made any mistakes in their methods. My concerns are in the interpretations of their findings.
This matters, because it implies that the faults of trustworthiness in our health care system can be linked in large part to a certain event, one that occurred decades ago. In response to this concern, the authors wrote to me: “There is nothing in our current study that suggests we are assigning full blame to a single event. In our abstract, we highlight that our estimates imply the disclosure can explain about 35 percent of the 1980 life expectancy gap between older black and white men.”
Still, some think this leap remains a stretch. I spoke to Susan M. Reverby, a professor of women’s and gender studies at Wellesley College, and one of the foremost experts on the Tuskegee study.
“I think that this study makes it look like the reason for mistrust happened a long time ago,” she said. “But in cases like this, the use of the term ‘Tuskegee’ is often raised as a metaphor for structural racism. That is what is at issue, not the Tuskegee study itself.”
Alice Dreger, a historian of medicine and science, said in an email to me: “African-Americans who distrust the health care system see plenty of reasons all around them to do so. They don’t have to look back 40 years.”
Mistrust in the health care system has multiple factors. It can come from huge lapses in ethics, like the Tuskegee study, but it can also come from the daily ways in which the system treats some people differently than others. It can even come from small missteps in the interpretation of results. The causes of the disparities we see are systemic, and would probably exist even without Tuskegee.
We should be careful about assigning blame to a single incident in the past, ignoring the many other issues that existed then, and still exist today.
To Learn More:
Tuskegee and the Health of Black Men (by Marcella Alsan and Marianne Wanamaker, National Bureau of Economic Research) (pdf)
U.S. Public Health Service Syphilis Study at Tuskegee (Centers for Disease Control and Prevention)
Should U.S. Compensate Guatemalan Victims of American Medical Experimentation? (by Noel Brinkerhoff, AllGov)
- Top Stories
- Unusual News
- Where is the Money Going?
- Controversies
- U.S. and the World
- Appointments and Resignations
- Latest News
- Trump Renames National Football League National Trump League
- Trump to Stop Deportations If…
- Trump Denounces World Series
- What If China Invaded the United States?
- Donald Trump Has a Mental Health Problem and It Has a Name






Comments