Fraudulent “Upcoding” Costs Medicare Advantage $2 Billion a Year
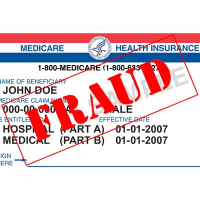 (graphic: Steve Straehley, AllGov)
(graphic: Steve Straehley, AllGov)
A new study has found that some Medicare Advantage plans make their patients seem sicker than they are in order to overbill the federal government to the tune of $2 billion a year.
Medicare Advantage plans are run by private insurance companies. Some of those eligible for Medicare choose them because they offer more features than the traditional fee-for-service plan administered by the federal government. The plans are paid for by the government partly on the basis of risk scores which reflect a patient’s health, according to Modern Healthcare.
The study (pdf), by University of Texas Professor Michael Geruso and Harvard Medical School research fellow Timothy Layton, says enrollees in Medicare Advantage plans have 6% to 16% higher diagnosis-based risk scores, called “upcoding,” than the same enrollees would have had if they were in traditional Medicare.
As a result, not only are the plans more profitable for the insurance companies, the extra money allows them to offer more benefits to enrollees which make them more attractive than regular Medicare.
Geruso cautioned, however, that not all upcoding is fraudulent. “There’s a notion that differences in coding come up because insurers are gaming the payment system,” Geruso told Modern Healthcare. “While I think there’s some of that going on, there are also probably some differences in models of managed care that result in different diagnosis codes being assigned.”
Geruso pointed out that there is similar risk-coding in the health exchanges set up as part of the Affordable Care Act. Insurers in those programs who more aggressively upcode their enrollees can make more money and offer more incentives to patients to enroll in their plans.
-Steve Straehley
To Learn More:
Upcoding In Medicare Advantage May Cost Government $2 Billion A Year (by Lisa Schencker, Modern Healthcare)
Upcoding: Evidence From Medicare On Squishy Risk Adjustment (by Michael Geruso and
Timothy Layton, National Bureau of Economic Research)
Overbilling by Doctors and Hospitals Costs Medicare a Billion Dollars a Year (by David Wallechinsky and Noel Brinkerhoff, AllGov)
- Top Stories
- Unusual News
- Where is the Money Going?
- Controversies
- U.S. and the World
- Appointments and Resignations
- Latest News
- Trump Orders ICE and Border Patrol to Kill More Protestors
- Trump Renames National Football League National Trump League
- Trump to Stop Deportations If…
- Trump Denounces World Series
- What If China Invaded the United States?






Comments